“Women who seek to be equal to men lack ambition.”
Timothy Leary
Mental illness is more common in women than in men. Elevated prevalence rates among women may be attributed to many factors, including female biology, an often overlooked variable in traditional mental health research and emerging psychedelic research.
Ovarian hormones may impact the serotonin reuptake process, a key biological target in psychedelic medicine. Estrogen, a fluctuating ovarian hormone, has been shown to increase the density of 5-HT2A receptors in female rat studies, and recent research on premenstrual dysphoric disorder suggests an increase in serotonin transporter density during the luteal phase of the menstrual cycle.
“With 5-HT2A thought to underlie the psychoactive effects of psychedelics, these findings suggest that when a woman's oestrogen is at its highest, psychedelic effects may be more potent. This suggestion could be important for women when deciding what dose of a psychedelic substance to take during different times of the month.” - How Psychedelics Interact with Hormones, HYSTELICA
Understanding the role of ovarian hormones in psychedelic research isn’t a niche research question, it’s required to calculate recommended dosage and to ensure the safety of the majority of patients that may access psychedelic medicine, who are women.
Because female biology may enhance the bioavailability of psychedelic medicines, not adjusting for sex in psychedelic research data may result in recommended dosages that are too low for men and too high for women.
Women are almost twice as likely to experience adverse drug reactions compared to men. A recent analysis found that most drugs currently in use were approved using clinical trials conducted on men, which likely contributes to increased adverse reactions in women.
“Men and women may be different in the way they respond to certain drugs. The pharmacodynamics (what the drug does to the body) can be affected by many factors, including sex hormones, which can fluctuate due to menstruation, pregnancy, menopause, [and] oral contraceptives.” - Pire-Smerkanich, Healthline
To date, there is little to no data on psychedelic medicines and ovarian hormones. This research gap leaves the majority of mental health patients in the dark regarding potent biological factors that may interact with psychedelic medicines.
Given the history of adverse drug reactions in women, the emerging psychedelic medicine industry has an opportunity to enhance and protect the integrity of the safety profile for psychedelic medicines.
Part 1. Prevalence of Mental Illness in Women
Mental illness is more common in women than in men. Some mental health conditions like post-partum depression, premenstrual dysphoric disorder and menopause related mental health impairments are directly related to female biology and cannot be diagnosed in men, a key factor when considering overall prevalence rates.
Women are twice as likely to develop post-traumatic stress disorder than men and more women develop major depressive disorder than men. The underlying cause for this disparity is likely a result of multiple factors including sexual violence, domestic violence, environmental stressors, cultural norms, female biology and men seeking care less often than women.
Women are More Likely to Seek Care for Mental Health
An analysis performed in 2020 showed that 51% of females with a mental illness received mental health treatment, while only 37% of males received treatment.
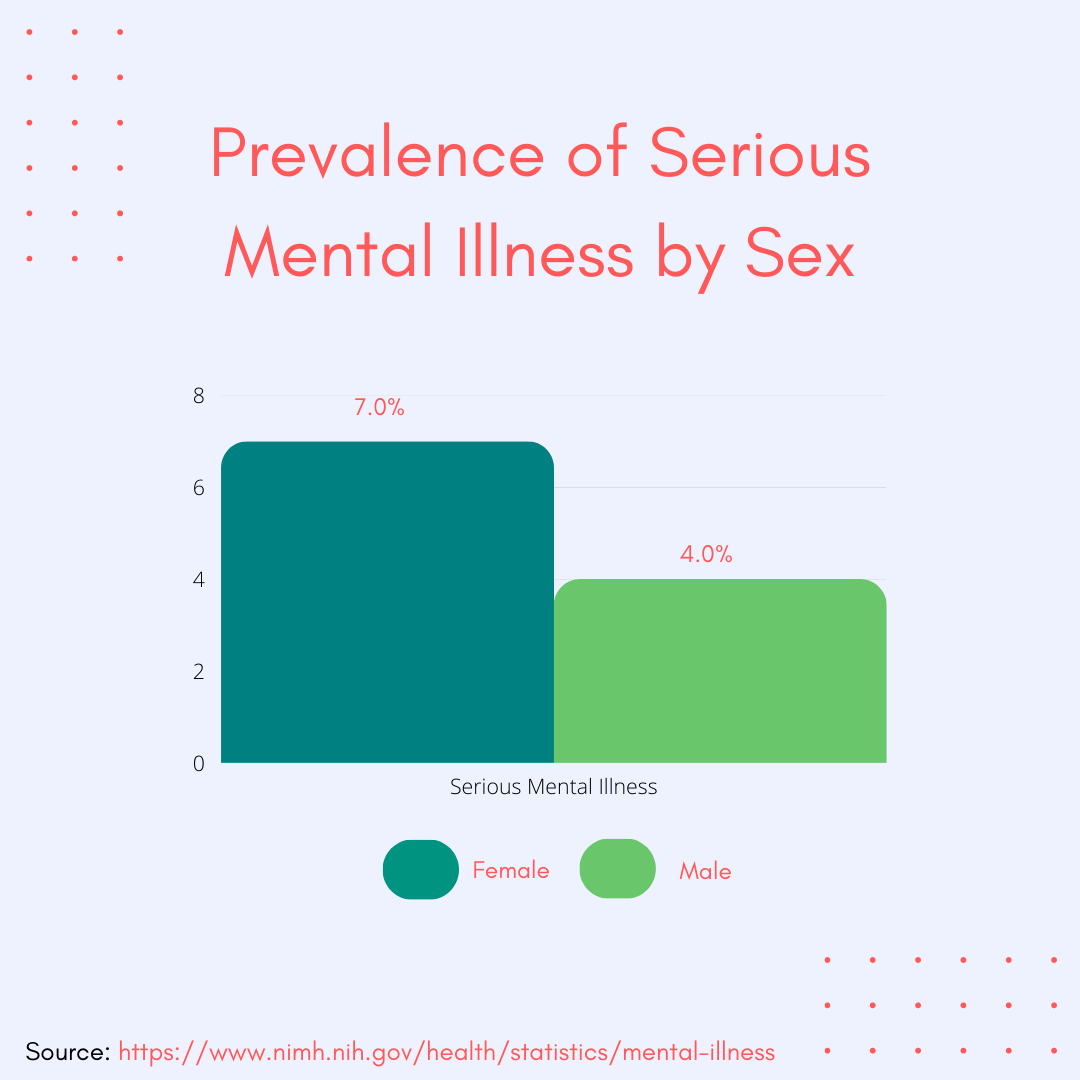
This statistic is often cited to demonstrate that men are less likely to seek care than women. While this is likely a factor, prevalence rates for serious mental illness is also higher in women - 7% vs. 4.0% - which may contribute to women seeking care more often than men.
Premenstrual exacerbation may also be a factor in the elevated severity of mental health conditions in women. A large study on major depression found that over 60% of women with the condition experience worsening of symptoms during the luteal phase of the menstrual cycle.
The luteal phase is roughly the two-week window before a period begins. The luteal phase starts after ovulation and ends with menstruation if the egg is not fertilized.
Part II. Premenstrual Conditions
Premenstrual Dysphoric Disorder, or PMDD, affects an estimated 4.2 million women in the US alone and the prevalence rate is comparable to men in the US with diagnosed PTSD, which includes both veterans and male civilians.
The rate of suicide attempts in PMDD patients is elevated compared to major depression and PTSD (34%, 31%, 27%), respectively. Symptoms overlap with both PTSD and major depression and can include suicidal ideation, depression, anxiety, sensory sensitivity, derealization, dissociation, anger and emotional lability during the luteal phase of the menstrual cycle.
While no clinical research has been done on psychedelics and premenstrual conditions, independent research is currently being conducted on PMDD and psilocybin mushrooms, and a growing number of case studies demonstrate therapeutic potential.
Given the overlap in symptoms with PTSD and major depression, understanding how ovarian hormones produce mental health symptoms in PMDD patients may help psychedelic scientists and researchers better understand the biological mechanisms responsible for how psychedelics work.
While serotonin is often referred to as a neurotransmitter, it also acts as a hormone. This dual action chemical phenomenon also occurs with estrogen and progesterone - ovarian hormones that act as neurotransmitters.
In the case of PMDD and premenstrual exacerbation, estrogen and progesterone may act as neurotransmitters rather than hormones to interact with the serotonin system.
Because female specific mental health conditions are understudied and societal awareness is lacking, PMDD is frequently misdiagnosed and underdiagnosed. It’s likely that some women seeking care for major depression and / or PTSD may actually have PMDD or premenstrual exacerbation.
Given the potential increase in serotonin transporter density in PMDD during the luteal phase of the cycle, screening for this condition and considering dose and timing before administering psychedelic medicines to women is critical.
Part III. A History of Harm Reduction for Women
Because female biology may interact with psychedelics in an unknown way, and there is a history of adverse drug reactions in women, the psychedelic industry has an opportunity to improve the safety profile for psychedelic medicines and avoid past mistakes made in traditional medicine.
Historically, women were excluded from clinical research which likely contributes to the increase in adverse drug reactions when compared to men. In 1977, the Food and Drug Administration recommended excluding women of childbearing age from clinical trials due to the complexity of female biology, and a series of birth defects; in particular, the experimental drug thalidomide, which resulted in extreme limb deformities in babies born to mothers who took the drug while pregnant.
Excluding pregnant women from experimental drug trials is a logical policy given the risk of birth defects, but the FDA recommendation did not adjust for women that weren’t sexually active, were using contraceptives or had partners with vasectomies.
The result of this policy was an overly broad exclusion of reproductive-aged female participants in clinical trials until 1993, when Congress wrote Women and Minorities as Subjects in Clinical Research into law.
The law requires that NIH-funded studies include female participants and that trials should be designed to enable analysis of how variables being studied may impact females differently than males.
Many of the pharmaceuticals prescribed today were approved by the FDA prior to 1993 and were brought to market for both men and women without female representation in early-stage clinical trials.
In the case of Ambien, a commonly prescribed sedative approved by the FDA in 1992, recommended dosage was not adjusted for women until 2013, two decades after the drug was first prescribed, following reports of adverse drug reactions including cognitive deficits and an increase in traffic accidents the day after taking it.
The FDA issued a sex-based dose adjustment for Ambien in 2013, lowering the recommended dose for women citing safety concerns from adverse drug reactions.
Following the dose adjustment, NIH Director Francis Collins established the Sex as a Biological Variable policy in 2016 requiring the study of ‘Sex as a Biological Variable’ in preclinical, biomedical research such as mice studies.
While one would assume that sex as a biological factor is basic, no-shit science and should have always been a factor, biomedical research focuses heavily on male animals and cells.
As a result, more women are being recruited and encouraged to participate in clinical trials, and more female animals and cells are being used in biomedical research. Still, research outcomes and related data are not often adjusted by sex. The failure to adjust for dosage and outcomes based on sex may negatively impact both men and women.
“A 2018 review of 107 NIH funded randomized control trial studies that enrolled both men and women found that only 26% reported even one outcome by sex or included both sexes as a covariate [7]; 72% simply did not include sex in their analyses. NIH policies mandated over a quarter century ago have yet to yield the intended increases in reporting by sex.”
Zucker, I., Prendergast, B.J. Sex differences in pharmacokinetics predict adverse drug reactions in women. Biol Sex Differ 11, 32 (2020). https://doi.org/10.1186/s13293-020-00308-5
Understanding the history of female biology in clinical research helps psychedelic researchers avoid past mistakes made in traditional drug development processes.
Psychedelic medicines have an impressive safety profile when compared to many pharmaceuticals, but research on their interaction with ovarian hormones is largely unexplored. This research is vital to protect the integrity of the safety profile of psychedelic medicines.
You can support this research by signing the Open Letter to MAPS.
Part IV. Healing Isn’t a Zero Sum Game
“Early research on the use of psychedelics to treat trauma has focused primarily on combat veterans, a vast majority of whom are men. Without careful attention paid to make psychedelic therapy safe and inviting for women and people who are genderqueer or transgender, norms which make it safer for cisgendered men to participate in such healing will only intensify.”
— Betty Aldworth, Director of Communications and Marketing for MAPS
Support for new PTSD treatments for veterans is bi-partisan and generally popular with constituents, leading to an increase in political motivations for psychedelic research and funding.
As a result, early research on PTSD and psychedelics focused heavily on combat veterans who are predominantly male. The association of PTSD and veterans has the potential to overshadow the needs of the majority of patients diagnosed with PTSD, who are female civilians.
While early research may be viewed as a step in the wrong direction for women’s health, bi-partisan support for psychedelic medicine and open conversation about trauma in the veteran community has the potential to make a significant impact for the lives of millions of PTSD patients who are predominantly women.
In addition, male trauma does not only impact men; it is distributed throughout families and communities impacting countless mothers, daughters, wives and partners.
Female specific mental health conditions do not only impact women; they are distributed throughout families and communities impacting countless fathers, sons, husbands and partners.
While combat veterans are predominantly male, the rate of female veterans is steadily increasing demonstrating a need to better understand trauma and female related mental health conditions in women veterans.
When both men and women are given the safe opportunity to heal together, the results are compounding, increasing the quality of life for both parties and enhancing the communities in which we all live.
The prevalence of mental illness in women may be attributed to many factors including female biology, which is often overlooked by researchers, scientists, industry leaders, entrepreneurs and investors who are predominantly male.
However, for the ones that can look beyond their own lens of the world to see a bigger picture, an opportunity exists to protect the integrity of the safety profile of the psychedelic medicine industry in general, and contribute to the lives of millions of mental health patients who are currently underserved by traditional healthcare and psychedelic medicine.







Great data and insights. I think most people consider only their weight with regard to doses, and wouldn’t have thought that hormonal/menstrual activity would affect the bioavailability of a compound. But it’s rather obvious once pointed out.